Table of Content
Early identification of this diagnosis, as well as the sub-type of priapism, allows for rapid initiation of indicated treatments. Thus, collaboration between emergency medicine physicians and urologic specialists is imperative to the provision of appropriate, timely care. Early penile prosthesis placement in management of acute ischemic priapism. First-lineThe treatment of each acute episode is similar to that of low-flow priapism.Drug therapyHormonal therapies and/or antiandrogens or phosphodiesterase type 5 inhibitors, depending on the patient’s medical profile. Sickle cell patients – This group of patients may require a specific regime of therapy to treatment their sickle cell disease, including oxygenation, hydration, alkalinization, analgesia and exchange transfusion. When an erection lasts for too long, this oxygen-poor blood can begin to damage or destroy tissues in the penis.
Differentiating low-flow from high-flow priapism is critical because treatment for each is different. Your doctor might review your medical history and perform a physical examination to help determine the cause of priapism. Once the emergency is resolved, further blood tests might be prescribed to assess your blood health. Intermittent priapism is a type of low-flow priapism characterised by repeating episodes of painful, prolonged erections. However, patients who suffer from blood disorders, especially sickle cell disease, may develop priapism. Some blood, metabolic, or nervous system disorders and medications put patients at higher risk.
What is priapism?
In cases of prolonged erections resulting from in-office intracavernosal erectogenic injections, the treating physician should make appropriate efforts to achieve adequate detumescence prior to dismissal from the office. Patients should also be counseled as to appropriate management strategies if a fully rigid erection were to recur after leaving the office. A persistent erection following iatrogenic- or patient self-administration of erectogenic medications into the corpus cavernosum represents a distinct pathology when compared to acute ischemic priapism or NIP. As such, the natural history and treatment protocols for a prolonged, iatrogenic erection must be differentiated from guidelines and protocols for true priapism. Recurrent or stuttering priapism, a form of ischemic priapism, is an uncommon condition.
However, the longer medical attention is delayed, the greater the risk of permanent erectile dysfunction. After the physical exam is complete, the doctor will take a blood gas measurement of the blood from the penis. During this test, a small needle is placed in the penis, some blood is drawn, and then it is sent to a lab for analysis. This provides a clue to the type of priapism, how long the condition has been present, and how much damage has occurred. Nonischemic or "high-flow" priapism is rare and usually results when an artery in the penis ruptures due to penile trauma or perineal injury, causing an influx of blood to flow in.
Guideline Statements
When body of evidence strength Grade C is used, there is uncertainty regarding the balance between benefits and risks/burdens; therefore, alternative strategies may be equally reasonable, and better evidence is likely to change confidence. Level B evidence may include observational studies rated as low quality if findings are consistent and of a strong treatment effect. Panelists can therefore make a stronger statement based on this evidence. In instances where evidence for a given question is rated as level C, this does not mean that the panel cannot make a statement based on the evidence, particularly if findings from included studies are not substantially different.
Normally if you see then many men suffers from erection problem. They actually don’t know how it occurs and what are the reasons behind this low erection.
What are the causes and risk factors of priapism?
The decision to intervene in the time-period between 1 and 4 hours would depend on several clinical factors which are discussed in greater detail below. Proximal shunts are optional for the surgeon, based on clinical judgment and comfort level. In general, it is the Panel’s opinion that proximal shunting represents a historical procedure and has largely been replaced by distal shunts with tunneling procedures.
The range of reported recurrences also varied widely (0-100%), which underscores the poor reliability of the data overall. Embolization of visualized fistulae or similar vascular anomalies represents a viable therapeutic option in men with NIP. Success rates of embolization in appropriately selected individuals remain high, however, as with all interventions, embolization carries risks of potential adverse effects, including ED, recurrence, and primary failure, among others. In a patient with diagnosed non-ischemic priapism, the clinician should consider penile duplex ultrasound for assessment of fistula location and size. These should never be used in SCD patients as they may worsen painful events by precipitating intravascular sickling. Clinicians may utilize penile duplex Doppler ultrasound when the diagnosis of acute ischemic versus non-ischemic priapism is indeterminate.
Priapism treatment
Searches identified 4117 potentially relevant articles, and 3437 of these were excluded at the title or abstract level for not meeting inclusion criteria for any key question. Full texts for the remaining 680 articles were ordered, and ultimately 203 unique articles were included in the report. When sufficient evidence existed, the body of evidence for a particular treatment was assigned a strength rating of A , B , or C , and evidence-based statements of Strong, Moderate, or Conditional Recommendation were developed. Additional information is provided as Clinical Principles and Expert Opinions when insufficient evidence existed. Priapism is an often painful penile erection that lasts four hours or more.

The Urology Care Foundation is a driving force in the discovery of new treatments, because we invest in the next generation of researchers. If you think that you are experiencing priapism, you should not attempt to treat it yourself. This temporary device is implanted into the penis to help reroute the trapped blood so that circulation can return to normal. We follow a strict editorial policy and we have a zero-tolerance policy regarding any level of plagiarism.
Whether you see a urologist or an emergency room provider, the initial aim of an evaluation to resolve an enduring erection is to distinguish which type of priapism is at play. Patients struggling with recurrent priapism sometimes also suffer, or have suffered, from ischemic priapism. After approximately four hours, when the environment becomes ischemic enough, patients perceive pain, he said. The ischemic variety tends to be idiopathic, or without a known cause, and occurs most often. A case of ischemic priapism must be managed quickly given the severe consequences of waiting, Akakpo said.
This can help your doctor diagnose blood disorders, cancers, and sickle cell anemia. The Panel recommends that the clinician perform repeat embolization in patients who are refractory to embolization. This should be done in the context of shared decision making after the patient is aware of the surgical options. Furthermore, while fistula ligation has historically been performed, it is an outdated procedure and there is inadequate evidence to quantify the benefit of the procedure. The Panel recommends this approach, as it is likely to be more effective and safer than an attempt at surgical ligaton, given the lack of experience in the latter approach for most urologists and the poor data supporting ligation. PDUS may be performed in a non-urgent fashion in a patient with NIP to help with screening for anatomical abnormalities and identification of cavernous artery fistula or pseudoaneurysm location and size.
Here we explore the treatment options for priapism, as well as some of the more common causes. It is often unrelated to or continues long beyond sexual activity. It can be a serious condition due to the risk of permanent tissue damage. But the longer you go without medical care, the greater your risk of lasting problems getting and keeping erections.
You might get fear about priapism and might opt for cold ice pack to apply on penis tip just to get relax but you should never do it. While you are suffering from the condition, applying penis can make the condition worse. Generally many few people take warm showers and if you don’t take warm showers then start taking it. Because it has proved that men suffering from priapism can be cured by taking warm showers. You can continue having sexual activities or masturbate while you are on priapism because it has no such effect on erection. I think you already know what stress can affect your sexual life, so why to take stress in life?
How is priapism treated?
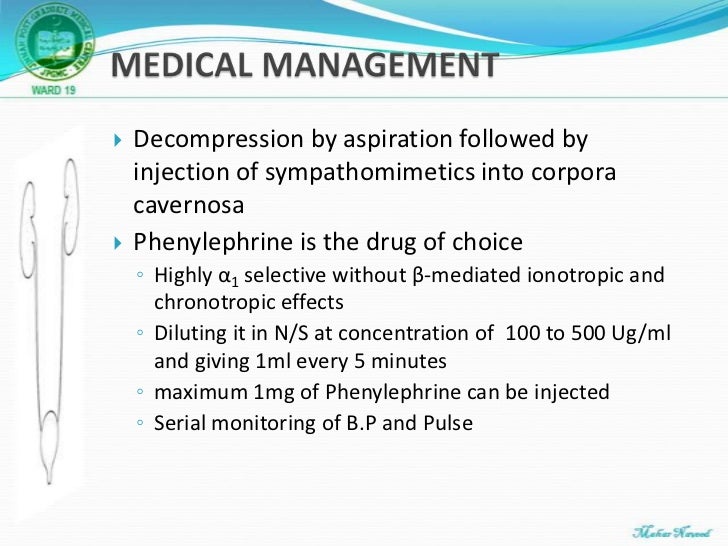
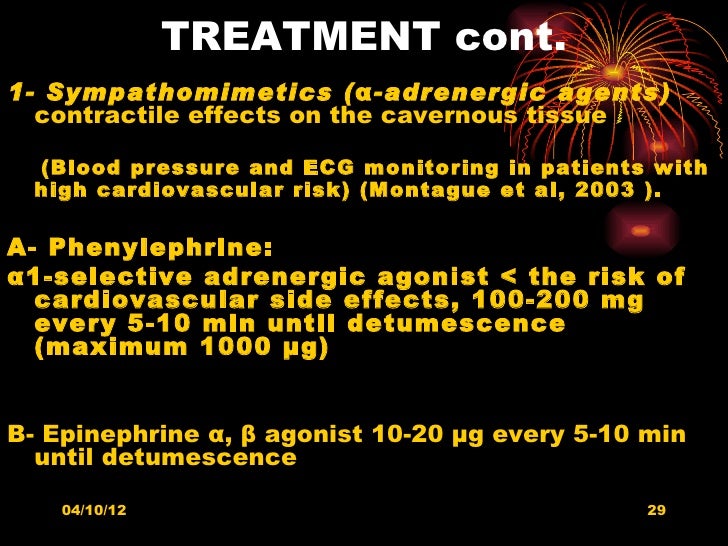
However, this should not be considered the gold-standard approach, as there are currently no publications which have identified any method which is superior to another. Similarly, the decision as to when to stop performing aspiration/irrigation with phenylephrine will depend on clinical factors, including response to aspiration/irrigation and time since priapism onset, among others. In the absence of any rigorous data pertaining to the optimal duration of observation, the Panel suggest that a 4-week period is reasonable, unless the patient is severely bothered by the tumesced penis. This 4-week monitoring period will permit the clinician to define if the fistula has started to close, supporting a further period of close observation. After the 4-week mark, the patient’s fistula can be re-evaluated using PDUS; the patient’s sexual function and degree of bother can be further quantified.

No comments:
Post a Comment